Alzheimer's Disease Signs and Causes - Is it type-3 Diabetes?
It is well known that bad diets can trigger obesity and diabetes, but there is growing evidence that Alzheimer's disease may actually be a form of diabetes (type-3 Diabetes) triggered by poor diets high in sugar and fat, lifestyle issues and being overweight.
If so there is a huge time bomb of issues to deal with as diabetes and obesity are on the increase.
A recent study using rats, published in the Journal of Alzheimer's Disease, suggested that Alzheimer's diseasemay be triggered by the brain developing a resistance to insulin which in turn interferes with proper lipid (fat) metabolism.
Over time, this can cause a build up of lipids in the brain as plagues because the lipids are not absorbed properly. In rats interference with insulin metabolism caused increased stress and inflammation in the brain and produced symptoms similar to those of dementia.
If Alzheimer's disease is indeed type 3-Diabetes a different strategy will be required for prevention focused on finding a way to restore insulin responsiveness and ways of addressing the metabolic problems that cause the brain to produce the plagues in the brain.
Prevention strategies may need to focus on reducing the risks of diabetes and its link to diet and obesity.
The experimental study of rats in the published study produced the classic signs of dementia - the rats became disoriented and confused and were unable to navigate properly through mazes. The original New Scientist article details the findings and all the implications.
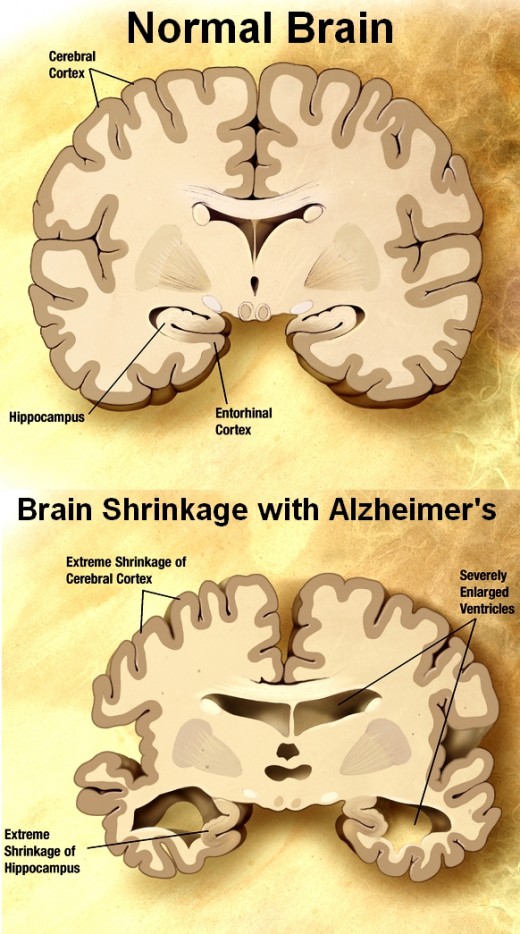
An examination of the rat brains showed that the areas in the brain linked to memory were studded with large numbers of bright pink plaques that resembles those that occur with Alzheimer's disease.
This problem in rats was induced by drugs that disrupted the normal way that brain cells respond to insulin. The hormone insulin is renowned for controlling sugar levels in the blood, but recent research has shown it also plays a key role in brain signalling.
Type 2 diabetes is characterized by the liver, fat and muscle cells failing to respond insulin. There is a decrease in the sensitivity to insulin in the tissues.
The recent research has suggested that people with type 2 diabetes or the early symptoms of insulin resistance, may be at risk of their brains showing similar resistance, causing changes in fat metabolism in the brain and brain function.
Recent research has shown that insulin plays the role of a'multitasker' in the brain: it helps neurons uptake glucose for energy, and it also regulates neurotransmitters, which are crucial for learning and memory.
Insulin is also important for maintaining the growth of blood vessels, which supply the brain with glucose and oxygen.
Consequently, lowering the level of insulin in the brain can immediately disrupt memory and learning functions. Conversely boosting insulin levels seems to improve these brain functions.
The origin of the plaques that is correlated with Alzheimer's disease is not completely understood. The substance beta amyloid is part of a larger protein that has a role in cell membranes in the brain and other parts of the body. It is also thought to have a number of other roles.
What causes the metabolic disruptions so that the protein fragments begin to clump and form into the plaques is unknown, but if the new research study is correct, the things that causes diabetes might be a trigger.
This new focus on insulin follows a realisation about the role it plays in the brain. Until recently, the insulin was solely regarded as a regulator of blood sugar, triggering cells in muscles, liver and fat cells to take up sugar from the blood and either use it for energy production or to convert the sugar into an energy reserve and store it as fat.
Type 2 diabetes typically involves hyperglycemia (abnormally high blood sugar levels) caused by defects in insulin secretion (impaired beta-cell function in the liver) and insulin sensitivity.
This decline in sensitivity means that liver and muscle tissues become resistant to insulin and higher levels are required to initiate normal functions.
These defects occur early in the course of the disease and can occur well before any diagnosis of diabetes.
Unfortunately, the beta-cell dysfunction that leads to impaired insulin secretion is often progressive, and eventually patients will require supplements of insulin to maintain glucose metabolism and other functions related to insulin.
The second trigger for diabetes - 'insulin resistance' may be caused by poor diet and obesity.
When people frequently gorge on sugary and fatty foods their insulin level peaks repeatedly and can remain at high levels for long periods of time. Muscle, fat and liver cells then stop reacting to normal levels of the hormone.
They becoming resistant to insulin. This means that cells in these organs don't take upfat and glucose in the blood.
Consequently, the pancreas has to work overtime to make more and more insulin to control the glucose levels which the body monitors.
The pancreas tries to meet the extra demand for insulin, but eventually gets exhausted, causing insulin levels to drop to abnormally low levels. It becomes a vicious cycle that interferes with the normal role insulin plays in the body.
Insulin, Excess Weight and Obesity
Weight gain appears to magnify the problem. Studies have shown that 80% of people with type 2 diabetes are also overweight or obese. Though the mechanism is still unclear, obesity >seems to trigger the release of inflammatory and metabolic stress molecules inside liver and fat cells that disrupt insulin action, leading to high blood glucose levels and, eventually, insulin resistance.
The new research suggests a similar process may lead to Alzheimer's disease, but this has yet to be confirmed. The suggestion is that constantly high levels of insulin, triggered by the fat and sugar content of the western diet, might over-stimulate the insulin related function in the brain, meaning that it isconstantly in a highly alert state.
Just as in the muscle and liver tissues the brain may begin to turn down its insulin signalling, becoming resistant to insulin and this may impair brain function and memory before leading to permanent neural damage. This process is insulin resistance in the brain that may also impair lipid metabolism causing plaques to accumulate.
In the study on rats a chemical was used to artificially increase insulin resistance and the results looked surprisingly similar to Alzheimer's, including the build-up of plaques. Various previous studies have shown a that disruptions to the insulin system can lead to the symptoms of Alzheimer's.
A study using rabbits showed that triggering diabetes created Alzheimer's-like brain changes in rabbits, including a sharp rise in the number of beta amyloid proteins. In another study, rats were fed a high fat diet for 12 months. This greatly impaired their ability to regulate insulin and caused to diabetes. Once again, this triggered high beta amyloid levels in the brain.
In another study a group of volunteers, who did not have diabetes, consumed foods that were high in saturated fat and sugar while a control group ate a diet low in saturated fat and sugar.
After only four weeks, the subjects on the high-fat and high-sugar diet had much higher levels of insulin in their blood and significantly higher levels of beta amyloid in fluid extracted from their spines.
The control group showed lower levels of both insulin and beta amyloid. It appears from this study that poor diets interfere with normal insulin functions in the brain and may trigger amyloid regulation and metabolism.
Although further research is needed is appears that obesity may be a major risk factor for diabetes and for dementia, with poor diets and processed foods playing a major role.
It is true that most people diagnosed with Alzheimer's have not been diagnosed with type 2 diabetes - though many show early-warning signs of insulin irregularities. Nevertheless the brain malfunction problems and metabolism changes may develop well before people are diagnosed with diabetes.
Conclusion:
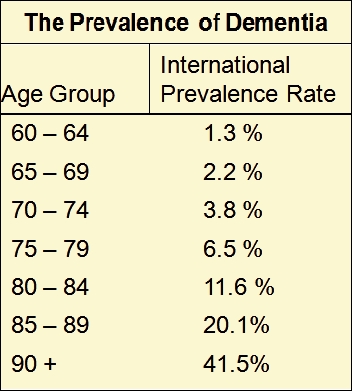
The new research is an early warning sign of a potential link between high fat and high sugar diets, type 2 diabetes and risk of dementia, which is already very high and growing.
In American, 19 million people have now been diagnosed with type 2 diabetes, while an additional 79 million are considered 'pre-diabetic', displaying preliminary signs of insulin resistance.
If Alzheimer's disease and type 2 diabetes do share a similar mechanism a major shift in treatment and prevention strategies may be warranted.
Alzheimer's Disease may in fact be type-3 Diabetes triggered in part by the Western Diet of processed foods rich in sugar and fat and unrelenting increase in body weight throughout the world.